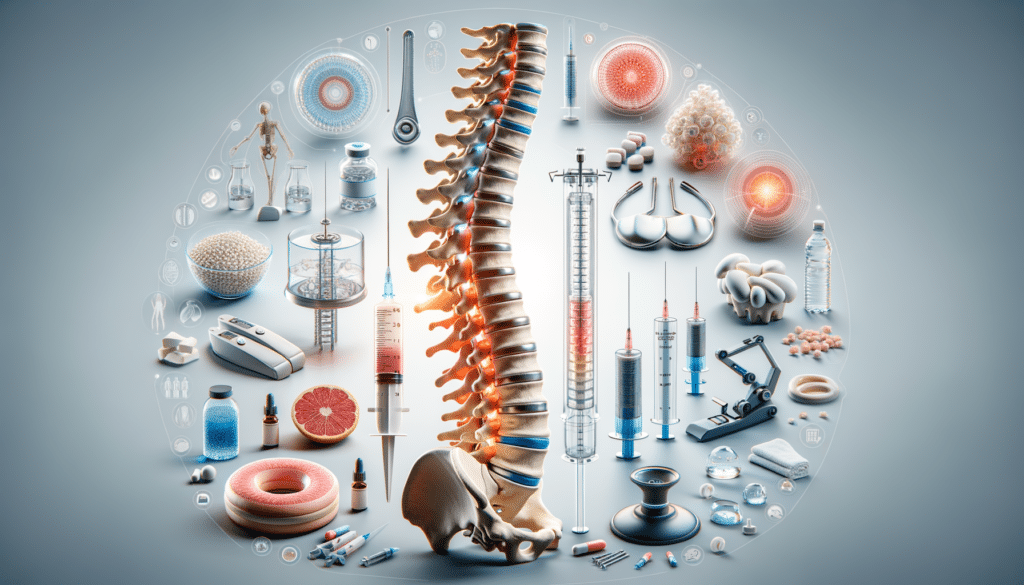
Understanding Spinal Stenosis: An Overview
Spinal stenosis is a condition characterized by the narrowing of spaces within the spine, which can exert pressure on the nerves traveling through the spine. This condition is most commonly seen in the cervical and lumbar regions of the spine. As individuals age, degenerative changes in the spine can lead to this narrowing, causing pain, numbness, and muscle weakness. Understanding the underlying causes and symptoms of spinal stenosis is crucial for effective management and treatment.
Spinal stenosis often results from age-related changes such as osteoarthritis, which leads to the formation of bone spurs. Other contributing factors include herniated discs, thickened ligaments, and spinal injuries. Symptoms vary depending on the location of the stenosis. In the lumbar region, symptoms may include lower back pain, leg pain, and difficulty walking, while cervical stenosis can cause neck pain, balance issues, and even bladder dysfunction.
Early diagnosis and intervention are key to preventing the progression of symptoms. Diagnostic tools such as MRI and CT scans are commonly used to confirm the presence and severity of spinal stenosis. Once diagnosed, a tailored treatment plan can be developed to address the specific needs of the patient.
Non-Surgical Treatments: A Conservative Approach
Non-surgical treatments are often the first line of defense against spinal stenosis, focusing on relieving symptoms and improving quality of life. These treatments are particularly beneficial for individuals with mild to moderate symptoms. Physical therapy plays a pivotal role, emphasizing exercises that strengthen the back and core muscles, improve flexibility, and enhance balance.
Medications such as non-steroidal anti-inflammatory drugs (NSAIDs) are frequently prescribed to reduce inflammation and alleviate pain. In some cases, corticosteroid injections may be recommended to provide temporary relief from pain and swelling. These injections are typically administered directly into the epidural space of the spine.
Other non-surgical options include lifestyle modifications and alternative therapies. Patients are encouraged to maintain a healthy weight, engage in regular low-impact exercises such as swimming or cycling, and consider chiropractic care or acupuncture as complementary therapies. These approaches aim to manage symptoms without the need for invasive procedures.
Surgical Interventions: When and Why
In cases where non-surgical treatments fail to provide adequate relief, surgical interventions may be considered. Surgery is typically reserved for individuals experiencing severe pain, significant neurological deficits, or loss of bowel or bladder control. The goal of surgery is to decompress the spinal cord or nerves by removing or reshaping bone and tissue.
Several surgical options are available, each tailored to the specific location and severity of the stenosis. Laminectomy, for instance, involves removing the lamina, or part of the vertebra, to create more space for the spinal cord. Foraminotomy enlarges the opening where nerve roots exit the spine, while spinal fusion may be performed to stabilize the spine after decompression.
While surgery can be highly effective, it is not without risks. Potential complications include infection, nerve damage, and blood clots. Therefore, a thorough evaluation and discussion with a healthcare provider are essential to determine the most appropriate surgical approach.
Emerging Therapies and Innovations
The field of spinal stenosis treatment is continually evolving, with new therapies and technologies emerging to enhance patient outcomes. Minimally invasive surgical techniques, for example, offer the benefits of reduced recovery times and minimized tissue damage. These procedures utilize smaller incisions and advanced imaging to precisely target the affected area.
Regenerative medicine is another promising area, with treatments such as stem cell therapy and platelet-rich plasma (PRP) injections showing potential in promoting healing and reducing inflammation. These therapies aim to harness the body’s natural healing capabilities to repair damaged tissues and improve function.
Moreover, advancements in imaging and diagnostic tools are improving the accuracy of spinal stenosis diagnosis, enabling more personalized treatment plans. As research continues, these innovations hold the promise of more effective and less invasive treatment options for individuals with spinal stenosis.
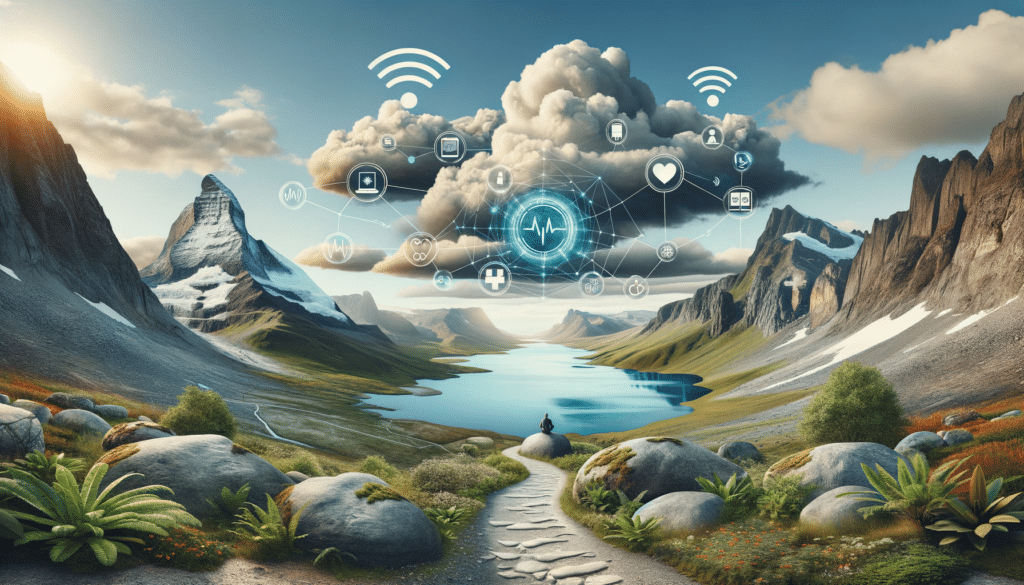
Living with Spinal Stenosis: Management and Support
Managing spinal stenosis is a lifelong process that requires a combination of medical treatment, lifestyle adjustments, and support. Patients are encouraged to adopt a proactive approach to their health, focusing on maintaining physical activity, managing stress, and seeking regular medical care.
Support groups and educational resources can be invaluable for individuals living with spinal stenosis. These platforms provide opportunities to share experiences, learn from others, and gain access to the latest information on treatments and therapies. Mental health support is also crucial, as chronic pain can significantly impact emotional well-being.
Ultimately, living with spinal stenosis involves finding a balance between managing symptoms and maintaining a fulfilling lifestyle. With the right combination of treatments and support, individuals can lead active and productive lives despite the challenges posed by this condition.